

What are the symptoms?
- Asymptomatic: Sometimes they do not cause any symptoms and you do not realise you have them.
- Bleeding – The bleeding is usually fresh blood and painless and occurs at the end of opening your bowels.
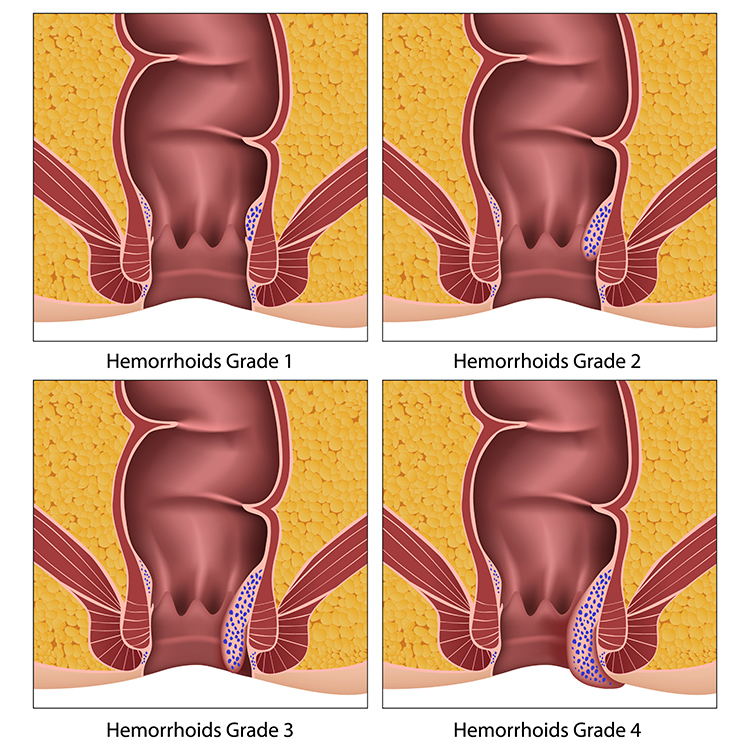
- Prolapse – As they get larger (Grade3/4) they can protrude out of the anal canal and give a sensation of a lump at the back passage which may cause discomfort, mucous discharge, anal irritation and itching.
- Pain – If the piles get thrombosed (blood clot), they can be extremely painful. The pain usually reaches a peak after 48-72 hours and then gradually goes away over 7-10 days.
Do I need any Tests?
Any bleeding from the back passage needs investigating and your GP will assess the need for further tests.
- Rectal examination – This a finger examination by a lubricated gloved finger to examine the back passage for lumps and bumps.
- Proctoscopy – Is a visual examination with a small instrument with a light to examine and grade the piles.
- Sigmoidoscopy/Colonoscopy – These are specialist tests to ensure that there is no other cause of bleeding from further up inside of the bowel (further info in relevant sections).
What treatments are available?
- Lifestyle
Most of the mild symptoms can be treated by simple changes to your lifestyle.- Avoid constipation by increasing fibre content in the diet or fibre supplements.
- Ensure adequate hydration to keep stools soft and easy to evacuate.
- Establish a regular toilet routine and avoid staring.
- Keep good anal hygiene by avoiding repeated wiping by harsh toilet paper which can cause micro-abrasions and make the itching worse. Gentle dabbing with most baby wipes or using a douche or showerhead and wiping with a cotton cloth.
- Avoid constipating pain killers if possible.
- Ointments and creams
Haemorrhoid creams or suppositories (dissolvable soft pellets that are placed inside the anus) are available over the counter and normally contain a local anaesthetic and a mild steroid to reduce irritation and inflammation. They should be used for only a few days, as they may cause, skin atrophy, contact dermatitis and sensitisation of the anal skin. - Banding of Haemorrhoids
Internal haemorrhoids Grade 2 can be treated by placing a tight rubber band at the base of the piles to cut off its blood supply causing it to shrink and eventually drop off. This is generally a painless procedure that can be performed in the clinic.
Surgical Options
If symptoms are not controlled by simple lifestyle changes or the piles are large you may need surgical treatment and need a General or regional anaesthesia.
- Haemorrhoidectomy
This is a surgical excision of haemorrhoids performed for large and prolapsing haemorrhoids. This is a painful procedure, however, there is a less chance of recurrence and may sometimes be the ideal procedure for a prolapsing painful haemorrhoid. Complications can include infection, secondary haemorrhage, urinary retention, abscess formation, faecal incontinence, fistula and anal stenosis. - Haemorrhoidal Artery Ligation
The procedure involves identifying the feeding haemorrhoidal vessels with a Doppler probe and cutting off the blood supply to the haemorrhoids by suture so shrinking them. The prolapsing haemorrhoid can then be hitched up back inside the anal passage.
More information on NICE and ACPGBI website
www.nice.org.uk
www.acpgbi.org.uk





 Youtube Channel
Youtube Channel